Essential Services: Activities and Recreational Therapy Professionals Making A Difference!
Compiled by Jeff Witman, CTRS, FDRT, Professor Emeritus, Applied Behavioral Sciences, York College of PA
On March 11, 2020 I had the privilege of speaking to the Lancaster Activity Directors Association's monthly meeting at Brethren Village. We greeted each other with handshakes and hugs, enjoyed a buffet lunch sitting 8 to a table, sang a song and practiced Tai chi as a group. Within a week these activities and many others were no longer happening in attendees' work places.
Covid 19 continues to have a profound effect on nursing homes and other healthcare facilities in Pennsylvania. In this edition of Dig It and the next (coming on October 5) four front-liners share their perspectives on responding to the virus.
Mary Schreiber, CTRS, Therapeutic Recreation Manager, Luthercare
As a Recreation Therapist in a long-term care facility that was sadly and significantly impacted by Covid-19, my world has been forever changed and is still changing. My role is now considerably different than it ever was and is now twofold: providing meaningful and purposeful activities to fight boredom and isolation, and keeping residents connected to people important in their lives. Thanks to a very dedicated Therapeutic Recreation team, we’ve been able to offer traveling activities to provide physical, social, intellectual, and spiritual opportunities. Video chats and window visits between residents and family members have become creative opportunities to engage as visitors sing, pray, and laugh together. Most important of all, we have ongoing open dialogue with our residents about the changes that are happening around them. As we move toward recovery and healing, there have been some bright spots along the way. We have seen resilience on display from our residents, a generation who already survived numerous hardships in their lifetime. As they cope with the feelings and emotions that come with restrictions on visitors and gatherings, they are again rising, this time with determination that COVID-19 will not define them.
Mary Ligon, PhD, CTRS, Associate Professor of Gerontology, York College and York Hospital
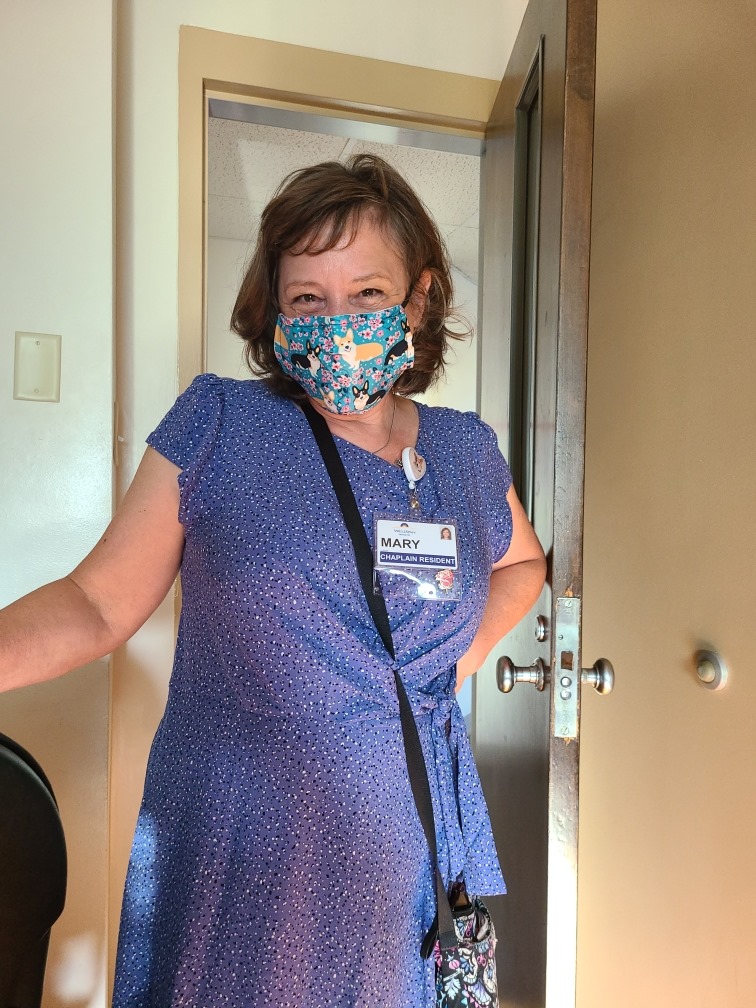
What: I was serving as a chaplain in a Medical-Surgical Hospital when COVID-19 occurred. In a hospital setting, chaplains meet the emotional and spiritual needs of patients, families, and staff. COVID-19 had a huge impact on the work of chaplains. Whereas before we went to patients' rooms to meet with them, now we were restricted to calling patients on the phone unless it was an end of life situation. This lack of personal contact was very hard on many patients. During one phone conversation, a patient said to me, "If I could choose a diamond ring or a hug, I'd take a hug right now. But I can't have either." For a period of time, no visitors were permitted into the hospital at all, except in the occurrence of end of life. This was an extreme hardship for patients and families alike. As we called patients on the phone, one of the most common concerns they expressed was their feelings of loneliness and isolation because they could not be with their loved ones while going through their hospitalization. Phone calls, FaceTime and Skype helped alleviate the loneliness to a degree but they did not replace the need for human contact. The stress felt by patients and families was passed along the staff which impacted them tremendously. This stress was on top of the stress staff were already feeling because of fears for their own well-being or fears of bringing something home to their families. Caring for the emotional and spiritual needs of the staff became a top priority for chaplains. As an example, I was invited by a Unit Manager to come at the shift change and pray for and bless the nursing staff on a medical unit one day. She explained how overwhelmed people were feeling. They seemed to truly appreciate this blessing. Additionally, the Spiritual Care Department began offering weekly prayer times via zoom for the staff so they could express their concerns, needs, and joys there. Eventually, the chaplains were permitted to return to visiting patients in-person. But now we do so with masks on and carefully using our PPE (personal protection equipment). It's a relief yet also brings new challenges and anxieties.
So What: In a hospital setting, people face crisis situations daily which brings out the need for emotional and spiritual support. COVID-19 heightened those anxieties. The most apparent lesson I learned from going through the time of COVID-19 in a hospital setting is that people need people and this need is never stronger than when faced with a crisis on top of a crisis. Modern technology is wonderful. Thank goodness for the old-school hospital phones that allowed us to converse with patients. Thank goodness for Video Chats that allowed patients to 'see' their loved ones. At the same time, I think we all became aware of how much we need in-person contact and human touch.
Now What: They say that what doesn't kill you makes you stronger. Perhaps we're a bit more resilient having faced the hardships that have come with COVID-19. Perhaps we appreciate technology in a new way. Most of all, I hope we appreciate the people in our lives and value being with them in good times and bad. COVID-19 brought many hardships and tragedies. I hope we can hold on to the valuable lessons that came with it.